Lymphedema: Supportive care - Patient Information [NCI]
This information is produced and provided by the National Cancer Institute (NCI). The information in this topic may have changed since it was written. For the most current information, contact the National Cancer Institute via the Internet web site at http://cancer.gov or call 1-800-4-CANCER.
What is lymphedema?
Lymphedema is swelling caused by a buildup of lymph fluid in the body between the skin and muscle. Lymph fluid is part of the lymph system, which plays a role in your body's ability to fight infection and disease. If you have cancer, the cancer or cancer treatment can disrupt the flow of lymph fluid and cause lymphedema (also known as secondary lymphedema). Lymphedema may arise soon after cancer treatment, or it may develop years after treatment has ended. Most often, it develops slowly over months or years. 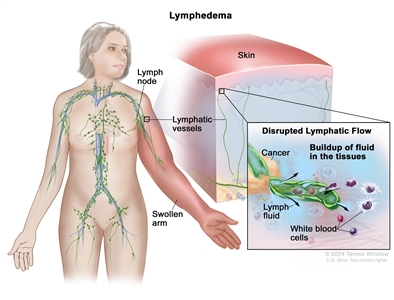
The lymph system helps the body fight infection and is made up of lymph nodes, lymphatic vessels, and organs that collect and carry lymph fluid through the body. If cancer or cancer treatment disrupts the flow of lymph fluid or damages lymph nodes and vessels, lymph fluid may build up and cause lymphedema.
Although lymphedema cannot be prevented, there are ways to lower your risk or keep lymphedema from getting worse.
Once lymphedema develops, it is a chronic condition that cannot be cured but can be treated to relieve swelling and improve your ability to function day to day. Lymphedema is easier to control when treatment starts early, so contact your doctor as soon as you notice heaviness, swelling, or other signs of lymphedema.
What causes lymphedema?
Anything that blocks or changes the flow of lymph fluid in the body can cause lymphedema. Cancer and cancer treatments can cause lymphedema when:
- cancer or a tumor blocks the flow of lymph fluid
- surgery for cancer disrupts the flow of lymph fluid
- radiation therapy causes scar tissue that blocks the flow of lymph fluid
Your risk for lymphedema depends on the type and location of your cancer and the treatments you have. Other risk factors for lymphedema include having an infection, healing slowly after surgery, having lymph nodes removed, past surgeries or radiation, having advanced cancer, and being overweight or having obesity. Talk with your doctor to learn about your risk of lymphedema.
Lymphedema and breast cancer
Treatment for breast cancer often involves surgery that removes one or more lymph nodes in the underarm area, increasing the risk of lymphedema. If you have been treated for breast cancer with radiation therapy or surgery, you may develop lymphedema in your hand, arm, or chest on the side of the body where lymph nodes were removed or damaged.
Lymphedema and other cancers
Lymphedema can occur anywhere in the body, but it most commonly affects an arm or leg. Some cancers—especially those that form in the abdomen or genital area—and their treatments are more likely than others to cause lymphedema because they are located near lymph nodes and vessels. Lymphoma, a cancer that affects white blood cells (part of the lymph system), can also cause lymphedema as white blood cells build up and block lymph flow.
The type of cancer you have can help predict where you may develop lymphedema.
- People with vulvar, vaginal, ovarian, endometrial, cervical, prostate, or colorectal cancer may develop lymphedema in the leg, genitals, or abdomen.
- People with head and neck cancer may develop swelling in the face, neck, or under the chin. You may also develop lymphedema inside your body, such as in your throat, in which case the lymphedema may not be visible.
Lymphedema can also develop after surgery for melanoma and sarcoma.
What are symptoms of lymphedema?
You may notice symptoms of lymphedema in an arm or leg or near where you had surgery or received radiation therapy. Signs and symptoms may develop slowly over time, so pay close attention to any slight changes. Contact your doctor if you notice any of these signs of lymphedema.
Signs and symptoms of lymphedema anywhere in the body
- A heavy, full, or tight feeling in the area where you had surgery or radiation therapy.
- Swelling. When you press on the swollen area, a dent may remain in the skin. However, as lymphedema gets worse, pressing on the swollen area may no longer leave a dent.
- Numbness or tingling in the affected area. Discomfort will worsen as lymphedema progresses.
- Discoloration and hardening of the skin in people with long-term, untreated lymphedema.
Signs and symptoms of lymphedema in the arms or legs
Lymphedema in your arm or leg may cause these additional signs and symptoms:
- a heavy, full, or tight feeling in your arm, leg, fingers, or toes
- swelling in an arm or leg that makes it appear larger than the other arm or leg
- difficulty moving your arm or leg
- weakness in your arm or leg
Signs and symptoms of lymphedema in the head or neck
Lymphedema in your head or neck may cause these additional signs and symptoms:
- swelling and a tight, uncomfortable feeling in your face, neck, or under your chin
- aching, tingling, pain, or numbness in your face, head, neck, shoulders, or ears
- difficulty moving your head or neck
- difficulty speaking, eating, swallowing, or breathing
- voice, vision, or hearing changes
Signs and symptoms of lymphedema in the genitals or abdomen
Lymphedema in your genitals or abdomen may cause these additional signs and symptoms:
- swelling in the genital area or abdomen
- difficult or painful urination
- pain during walking, sex, and other movements
Lymphedema and cellulitis
Cellulitis is a potentially life-threatening bacterial infection of the skin that is a common complication of lymphedema. People with lymphedema are at greater risk of cellulitis because skin in swollen areas is stretched thin, allowing easier entry of bacteria that thrive in fluid-rich areas of the body.
Some signs and symptoms of cellulitis are similar to those of lymphedema. Always check with your doctor about any skin changes or other symptoms you experience. Symptoms of cellulitis include:
- pain, tenderness, redness, and swelling in the affected area
- skin that feels warm to the touch in the swollen area
- fever
If you have a fever or other signs of cellulitis, call your doctor right away. If left untreated, cellulitis can become life-threatening. Your doctor can prescribe antibiotics to treat cellulitis.
How is lymphedema diagnosed?
You should watch for lymphedema signs and symptoms, such as tightness or swelling in an arm or leg, during and after cancer treatment. If you alert your doctor to swelling or other changes you have noticed, your doctor will examine the swollen part of your body. If swelling is affecting an arm or leg, they will compare the size of your swollen arm or leg with that of the other limb.
You may also have one or more of the following tests to help your doctor better understand the cause of swelling and what is disrupting the flow of lymph fluid:
- Ultrasound uses high-energy sound waves to examine how fluid, such as blood and lymph, is moving through the body. Doctors can use ultrasound to find a blood clot that might be the cause of swelling.
- Magnetic resonance imaging(MRI) uses a dye, magnet, radio waves, and computer to make a series of detailed pictures of areas inside the body. Magnetic resonance lymphangiography (MRL) is like an MRI, but it makes pictures of the lymph system. Doctors can use MRI and MRL to identify what might be blocking the flow of lymph.
- CT scan uses a computer linked to an x-ray machine to make a series of detailed pictures of areas inside the body from different angles. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography.
- Lymphoscintigraphy uses a small amount of radioactive glucose to allow doctors to trace the flow of lymph fluid and identify blockages.
- Perometry and water displacement are noninvasive techniques used to estimate the volume of a limb in people at risk of lymphedema.
- Bioimpedance spectroscopy is a noninvasive technique used to measure the amount of fluid in the body. It can help determine whether a person who does not have symptoms is in the beginning stages of lymphedema. This tool is sometimes used to help prevent lymphedema in people who are at risk.
Lymphedema stages
If you are diagnosed with lymphedema, your doctor will use a staging system to describe the severity of your lymphedema.
- Stage 0: The flow of lymph in the body is not moving as it should. You may or may not have symptoms.
- Stage I: The affected area is swollen and feels heavy. Pressing on the swollen area leaves a pit (dent) in the skin. Resting and elevating the limb can help reduce swelling at this stage.
- Stage II: The affected area is more swollen and may feel firmer than the area around it. Pressing on the swollen area does not leave a pit. Resting and elevating the limb no longer reduces swelling.
- Stage III: The affected area is extremely swollen and the skin feels hard and thick. You may also have decreased mobility and dry, blistered skin in the affected area.
How is lymphedema treated?
Treatments are available for managing the symptoms of lymphedema. Your health care team will talk with you about management techniques that can be done at home or under the supervision of a trained professional such as a nurse or a certified lymphedema therapist (CLT), a physical or occupational therapist trained to treat lymphedema. Treatments include:
Short stretch bandaging, compression wraps, leggings, or stockings
These can help move fluid around in your arms and legs to prevent it from building up. They may also be called compression garments. Your nurse or CLT will help you find garments that fit properly and will show you how to use them.
Manual lymphatic drainage
Manual lymphatic drainage, also called lymphatic drainage massage, involves gentle massage that helps move lymph fluid through the body. Lymphatic drainage is part of a treatment called complete decongestive therapy, which is managed by a CLT. Complete decongestive therapy may also include bandaging, exercises, and skin care to manage symptoms.
Compression pump
This is a device connected to a compression sleeve or sock that applies pressure intermittently to the arm or leg. The pumping action may help keep lymph fluid moving, preventing buildup in the limbs.
Surgery and other treatments
If lymphedema is advanced, your doctor may recommend surgery or another medical treatment.
- Lymphovenous bypass (also called lymphaticovenous anastomosis) is surgery that connects lymph vessels to a vein, creating a new path for lymph fluid to travel in the body.
- Lymphovenous transplant (also called vascularized lymph node transfer) is surgery that replaces damaged lymph nodes with healthy lymph nodes from elsewhere in a person's body, helping improve lymph flow.
- Liposuction removes extra fat in the affected part of the body and may improve lymphedema symptoms.
- Laser therapy uses light to stimulate new growth of lymphatic vessels, improve the flow of lymph fluid, and help repair skin affected by lymphedema.
Can I prevent lymphedema?
Although there is no way to prevent lymphedema, there are things you can do to lower your risk or keep it from getting worse. Your health care team may suggest the following things you can do at home:
- Protect your skin to prevent infection. Wear gloves when cooking and gardening to protect your hands from injury. Use lotion to prevent dry skin and cracks where bacteria can enter. If you get a burn or cut, ask your doctor about an antibacterial ointment to use. Always call your doctor if you notice redness or other signs of infection.
- Wear compression garments daily when you are up and moving around and at night as advised by your CLT.
- Learn manual lymph drainage techniques from your CLT that you can do at home.
- Exercise. Exercise is a natural pump for the lymph system. It can improve the flow of lymph fluid and keep the heart healthy, which may help treat lymphedema. Exercising may also help lower your risk of lymphedema. Talk with your doctor to find an exercise program that you enjoy and that is safe for you.
- Elevate the affected area when possible. If you have lymphedema in your arm, try to keep it raised above the level of your heart when sitting or resting. If you have lymphedema in your leg, elevate it while lying down by resting it on a pillow or rolled-up blankets.
- Stay at or get to a healthy weight. Being at a healthy weight can keep lymphedema under control.
- Avoid putting pressure on the affected area. Wear loose jewelry and clothes without tight bands or elastic. Avoid carrying handbags or other items with an affected arm. Blood pressure and blood draws should be taken using the arm without lymphedema.
- Avoid extreme heat and sun. High temperatures can make lymphedema worse. Use sunscreen and wear sun protection like hats and lightweight, long-sleeved shirts when spending time in the sun.
- Stay hydrated. Drinking plenty of water will help keep lymph fluid moving through the body.
- Reduce salt in your diet. Salt can make swelling worse by causing your body to retain fluid.
Talking with your doctor about lymphedema
As you prepare for a visit with your doctor, nurse, or social worker, consider making a list of questions to ask and adding these questions about lymphedema:
- Does my type of cancer or treatment put me at risk of developing lymphedema?
- What changes should I look for? Which ones should I call you about?
- If I am at risk of developing lymphedema, are there things I can do to prevent it from starting or worsening?
- How long after my cancer treatment might symptoms of lymphedema occur? Will I be monitored for early symptoms?
- What steps can I take to lower my risk for lymphedema?
- Are there special garments I should wear during the day or night to prevent or treat lymphedema?
- If I am diagnosed with lymphedema, is there a certified lymphedema therapist I could meet with?
Coping with lymphedema
The physical changes that result from lymphedema can affect your well-being. You may not be able to do the activities you once enjoyed or find clothes that fit properly. You may feel uncomfortable with the way you look and isolated from those around you. Working with a CLT is often the best way to manage and cope with lymphedema.
Side effects like lymphedema can be hard to deal with, both physically and emotionally. It's important to ask for support from your health care team. They can help you prepare for and make it through difficult times. Learn more about ways to cope with cancer including emotions that people with cancer often have and ways to adjust to daily life during cancer treatment.
For family members and friends who are caring for someone with cancer, you may find these suggestions for caregivers to be helpful.
Lymphedema research
Research is ongoing to discover new ways to prevent, diagnose, and treat lymphedema. Research studies called clinical trials help advance knowledge about lymphedema and other side effects of cancer and cancer treatment. Learn more at Clinical Trials Information for Patients and Caregivers.
To find NCI-supported clinical trials for lymphedema, go to Lymphedema Clinical Trials. Clinical trials supported by other organizations can be found at ClinicalTrials.gov.
Advances in cancer surgery and treatments are helping reduce the chances of lymphedema in people with cancer. For example, sentinel lymph node biopsy allows doctors to remove fewer lymph nodes when checking if the cancer has spread, decreasing the risk of lymphedema.
Related Resources
Last Revised: 2024-12-11
If you want to know more about cancer and how it is treated, or if you wish to know about clinical trials for your type of cancer, you can call the NCI's Cancer Information Service at 1-800-422-6237, toll free. A trained information specialist can talk with you and answer your questions.